Overview
Cancer is no longer a disease confined to the elderly. In recent decades, cancer diagnoses among young adults have surged by a staggering 80%, with colon cancer alone increasing by 13% since 2000. What was once a mid-to-late-life concern is now knocking earlier—and louder—on the doors of those under 50.
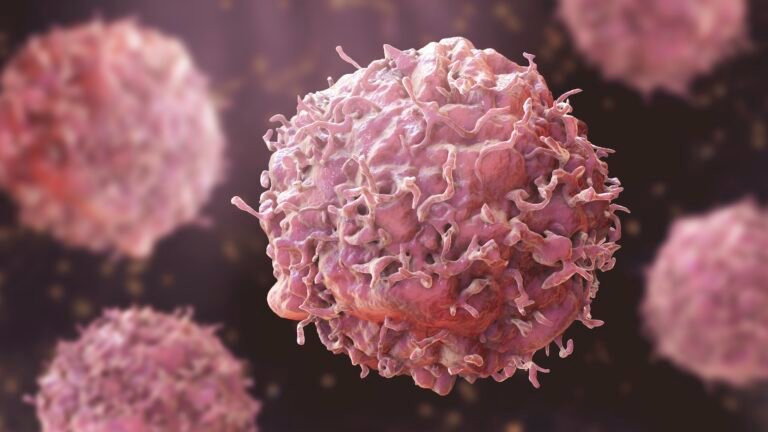
This shift has sparked concern across the medical community, especially as traditional treatments remain invasive, costly, and riddled with side effects. What’s emerging instead is a sharper, more promising approach: precision medicine—a field that tailors healthcare based on each individual’s genetic profile, lifestyle, and environment.
A Smarter Delivery Model: Patient-Centric, Tech-Enabled, and Decentralized
Karkinos uses a hub-and-spoke model, where centralized hubs offer advanced diagnostics and treatment, while localized “spokes” ensure basic care delivery in remote or underserved areas. This network approach ensures accessibility and affordability—key elements when addressing cancers in young adults, who may not have established financial stability or live near major hospitals.
What sets this model apart is how it integrates AI, real-time data, and cross-disciplinary collaboration. It’s not just about offering care, but offering the right care, faster and more efficiently.
As a healthcare commercialization expert and manager at the Stanford Pipeline, I’ve witnessed firsthand the growing traction of precision medicine. One company that exemplifies its real-world application is Karkinos Healthcare—an organization I’m unaffiliated with but whose innovative model caught my attention at the Stanford Precision Medicine Conference. Their approach offers a useful framework for what healthcare could (and should) look like moving forward.
Why This Matters for Young Adults
Healthcare organizations leveraging this model are uniquely positioned to:
Offer personalized treatment: Genetic and clinical data help tailor care to the individual, increasing success rates and reducing unnecessary treatments.
Drive cost-effective innovation: By integrating lab medicine, pathology, radiology, and genomics, diagnostics become streamlined. Redundancies are removed, diagnosis is faster, and the system becomes more affordable—especially crucial for younger patients.
Improve early detection: Big data can spotlight geographic or socioeconomic hotspots where cancer is emerging earlier. Targeted screenings and interventions can follow, helping catch cases early—when survival rates are highest.
Enhance R&D: Real-world data can accelerate research, leading to new therapies and use cases for precision medicine tailored to younger demographics.

The Strategic Challenge: Innovate, But Equitably
Of course, innovation brings new questions. How do we build business models that are ethically sound, financially sustainable, and scalable across diverse populations?
We need to answer:
What’s the value proposition? Is the value of patient data shared back with the communities it came from?
How will we pay for it? Especially in lower-income brackets, how can care be financed without creating new forms of disparity?
How do we deliver it? Beyond traditional clinics: mobile health units, telemedicine, and even home diagnostics must play a role.
Who’s responsible for producing it? Pharma, startups, and governments must cooperate to optimize the development and delivery of tailored therapies.
How do we protect patient data? Privacy must be preserved as data becomes more central to care decisions.
The Bottom Line: Precision Medicine Must Be a Systemic Shift, Not a Luxury
In 2021, the U.S. Preventive Services Task Force lowered the recommended age for colon cancer screening from 50 to 45. That’s a response to reality: cancer is trending younger. But lowering a screening age isn’t enough. We need a healthcare system that can detect risks before symptoms, treat patients as individuals, and evolve at the speed of data.
Diagnostic firms must move beyond selling tests to delivering actionable, personalized insights. Health providers must adopt connected, cost-efficient models. And governments must develop data policies and reimbursement structures that support proactive, not just reactive, healthcare.
In a world where cancer is becoming younger, will our healthcare systems mature fast enough to respond—with precision, equity, and urgency?