Rethinking Lung Cancer Prevention
Why CT Scans May Save More Lives Than Quitting Smoking Alone
Overview
For decades, public health efforts to combat lung cancer have focused almost exclusively on smoking cessation. But new findings from Dutch researchers are challenging that approach—particularly when it comes to older adults who have already spent decades smoking.
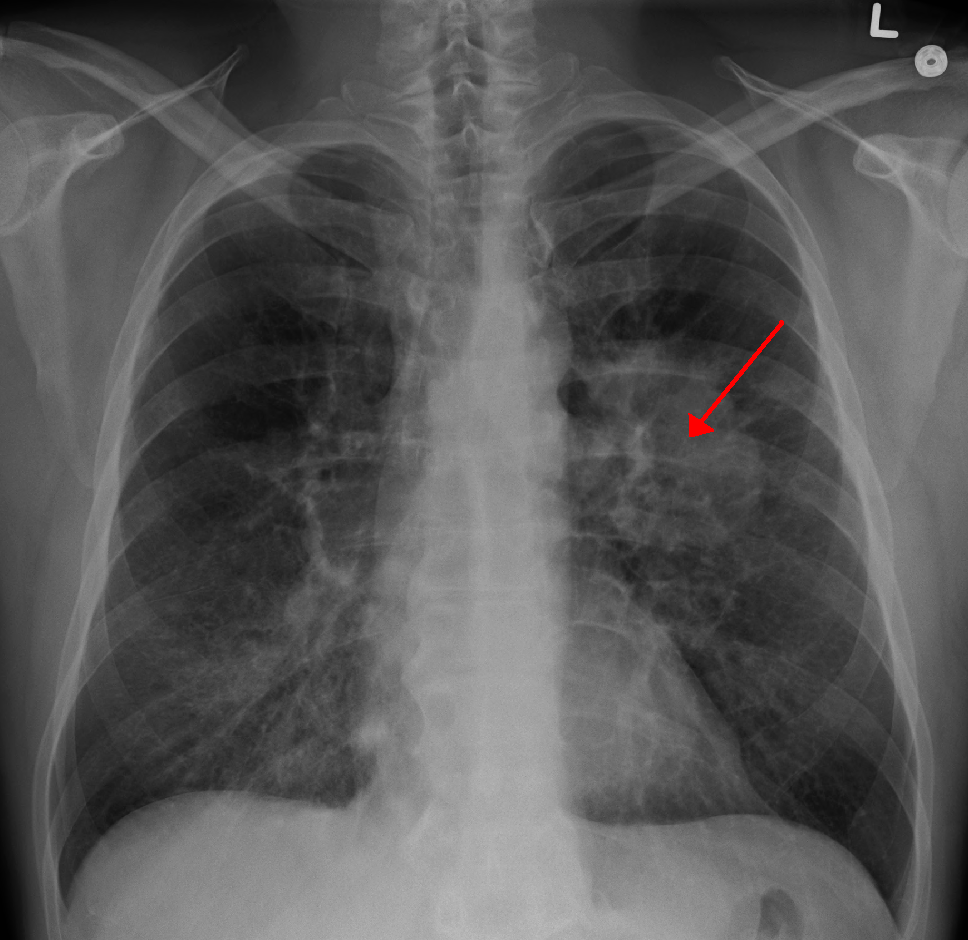
According to a large-scale study led by Erasmus MC University Medical Center in Rotterdam, early detection via low-dose CT scans is five to ten times more effective in extending life among smokers over 60 than quitting smoking at that stage. The logic is striking: by age 60, many long-term smokers are already in a high-risk group, and while quitting still offers some health benefits, the potential for developing lung cancer often remains. What truly shifts the odds in a patient’s favor is catching the disease before it advances.

A Global Public Health Recalibration?
The implications are significant—not just for physicians and patients, but for policymakers, healthcare leaders, and insurance providers. In the Netherlands, CT scans are currently only ordered when a patient presents symptoms. However, Associate Professor Carlijn van der Aalst, the study’s lead, is now calling for routine population screening among high-risk individuals, similar to existing Dutch protocols for cervical and colorectal cancer.
In the U.S., screening guidelines already exist: the U.S. Preventative Services Taskforce recommends annual lung CT scans for adults aged 50 to 80 with a 20-pack-year smoking history who currently smoke or quit within the past 15 years. But awareness and access remain uneven, especially among lower-income populations where smoking rates and lung cancer incidences are disproportionately high.
This is a critical inflection point. As newer, more targeted treatment modalities for lung cancer become available, their success often hinges on the stage at which the cancer is detected. According to the American Cancer Society, the five-year survival rate for lung cancer caught early is five times higher than if it’s discovered after metastasis.
This isn’t just a theoretical finding. The Dutch research—published in the New England Journal of Medicine—analyzed data from over 13,000 high-risk men and around 2,600 high-risk women. The results showed a significant reduction in lung cancer mortality among those who underwent CT screening compared to those who did not. Notably, women seemed to benefit even more from early detection than men.
A Global Public Health Recalibration?
The implications are significant—not just for physicians and patients, but for policymakers, healthcare leaders, and insurance providers. In the Netherlands, CT scans are currently only ordered when a patient presents symptoms. However, Associate Professor Carlijn van der Aalst, the study’s lead, is now calling for routine population screening among high-risk individuals, similar to existing Dutch protocols for cervical and colorectal cancer.
In the U.S., screening guidelines already exist: the U.S. Preventative Services Taskforce recommends annual lung CT scans for adults aged 50 to 80 with a 20-pack-year smoking history who currently smoke or quit within the past 15 years. But awareness and access remain uneven, especially among lower-income populations where smoking rates and lung cancer incidences are disproportionately high.
This is a critical inflection point. As newer, more targeted treatment modalities for lung cancer become available, their success often hinges on the stage at which the cancer is detected. According to the American Cancer Society, the five-year survival rate for lung cancer caught early is five times higher than if it’s discovered after metastasis.
The Cost-Saving Case
Beyond the human cost, there’s a powerful financial case for early screening. CT scans, while not inexpensive, can lead to long-term cost savings for healthcare systems by reducing the need for intensive, late-stage interventions. In an era where healthcare spending is under intense scrutiny, proactive screening may represent a smart and sustainable investment.
This is especially relevant as more countries, including Germany, France, and Italy, begin adopting similar demonstration projects. The momentum for a shift in preventive strategy is clearly growing.
A Strategic Opportunity for Leaders in Healthcare and Policy
For founders and leaders in healthtech, diagnostics, and policy-focused ventures, this shift opens up critical avenues for innovation. From mobile screening units to AI-assisted radiology and cloud-based population health monitoring, the tools for transforming early detection into standard care already exist—they just need integration and scale.
Likewise, for healthcare executives and policymakers, the challenge is to align incentives: between early detection programs, reimbursement models, and broader public health goals.
Are we ready to shift our healthcare models from reactive treatment to proactive detection—and are our systems equipped to make that transition equitably across income levels and geographies?